BULLOUS PEMPHIGOID
Introduction
Bullous
pemphigoid is a blistering skin disease which usually affects middle aged or
elderly persons. Symptoms: Bullae (large blisters, thin walled sacs
filled with clear fluid, greater than 1 cm. diameter) multiple usually located on the arms, legs, or trunk may also occur in the mouth may weep, crust over may appear deep below the surface of the skin may erode the skin, form ulcers or open
sores itching rashes mouth sores gums, bleeding.
Characteristically, crops of tense, fluid-filled blisters develop. They may
arise from normal-looking or reddened skin, often in body folds. Usually, the
skin is very itchy. Although sometimes pemphigoid is localized to one area such
as an ankle, it is usually widespread, and occasionally blisters develop all
over. The blisters of bullous pemphigoid
usually appear on the areas of the body that flex or move (flexural areas).
About one-third of persons with bullous pemphigoid also develop blisters in the
mouth. The disorder may occur in various forms, from no symptoms, to mild
redness and irritation, to multiple blisters. The cause is not known, but may
be related to immune system disorders. Bullous pemphigoid typically occurs in
elderly persons and is rare in young people. It is characterized by a pattern
of exacerbations and remissions. It may be without symptoms for 5 or 6 years,
then suddenly flare up.
How is it diagnosed?
The
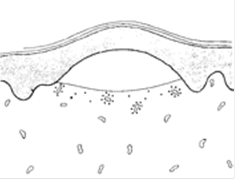
diagnosis is confirmed by taking a skin biopsy of a typical blister. Skin
lesion biopsy shows subepidermal blister (a blister that occurs beneath the
outer skin layer and the inner skin layers) and immunoglobulin deposits. Under
the microscope, the pathologist can see a split between the main layers of the
skin, the epidermis, and the dermis. This is thought to occur because
antibodies and white blood cells attack the membrane that holds the skin
together. It can be thought of as a type of allergy to one's own skin, i.e. one
of the autoimmune disorders.
What causes it?
Bullous
pemphigoid has been defined as a blistering disease of the elderly which often
starts with hive-like and itchy red lesions that later develops large tense
blisters. Pemphigoid is an affliction of the elderly, occurring predominantly
in persons between 60 and 75 years of age. However, the condition can occur in
the under forties and occasionally in children. There is no predilection for
any racial or geographical groups and there appears to be no predominant HLA
phenotype. The sex incidence is equal overall. Immune
phenomena are believed to be involved in the development of bullous pemphigoid.
The finding of autoantibodies to the epidermal basement membrane zone has confirmed that it is indeed a distinctive and recognizable
disease. Research data suggest a tentative mechanism for the pathophysiology of
the blister formation: Antibodies bind to the basement membrane zone and
activate complement. Complement components, especially C3a and C5a, attract
leukocytes and act as anaphylotoxins, degranulate mast cells, and release
inflammatory mediators. Leukocytes are attached to the basement membrane zone
and lysosomal enzymes from these cells result in damage to the basement
membrane and thus cause the blister formation. Bullous pemphigoid commonly
starts with a nonspecific rash on the limbs. This may precede the blisters
anywhere from one week to several months. Sudden generalization of the true
eruption of pemphigoid follows and most of the body may be affected within a
week. Bullous pemphigoid blisters are tense and dome-shaped obtaining a diameter
of up to 7 cm. They may arise in erythematous patches or plaques, or may
develop on otherwise normal-appearing skin. The blisters are tough and may
remain intact for several days. In some, the fluid is reabsorbed and the
epithelium settles back in place like a skin graft. Those which do rupture
leave erosions which heal rapidly, leaving mild post-inflammatory changes.
Sites of predilection include the inner aspect of the thighs, flexor surfaces
of the forearms, the axillae, the groin, and the lower abdomen. Mucous membrane
lesions occur less frequently and are usually confined to the mouth. Pruritis
is often present and is sometimes severe. Untreated pemphigoid runs a chronic
often self-limiting course over a number of years. Patients tend to be otherwise
in good health except for coincidental diseases or the ordinary infirmities
that may accompany old age.
How is it treated?
Treatment
is focused on relief of symptoms and prevention of infection. Corticosteroids
may help. They are given by mouth or by injection. Topical (applied to a
localized area of the skin) corticosteroids may also be used on early,
localized lesions. Antibiotics such as tetracycline or erythromycin may also be
given. For mild cases, Dr. Jacobs first tries a course of erythromycin,
tetracycline, or Dynabac antibiotics. Niacin (a B complex vitamin) may also be
used to manage this condition. If the pemphigoid is widespread, hospital
admission is usually arranged so the blisters and raw areas can be expertly
dressed, and the effect of treatment assessed. Infection also needs to be
treated. More severe cases of bullous pemphigoid are treated with steroid
tablets, usually prednisone. Corticosteroid therapy has lowered the mortality
considerably. Few deaths are attributable to the complications of treatment.
The dose is adjusted until the blisters have stopped appearing, which usually
takes several weeks. The dose of prednisone is then slowly reduced over many
months or years. As steroids have some undesirable side effects, we try to reduce
the dose as low as possible. If this is done too quickly, the blisters may
reappear. If the pemphigoid does not clear up with steroids alone, several
other medicines are useful. These include tetracycline antibiotics, dapsone,
azathioprine and methotrexate. Potent steroid creams may help clear up early
blisters. Treatment is usually needed for several years, but generally after a
few months it is possible to reduce the dose of prednisone to reasonably low
levels. In most cases the pemphigoid eventually completely clears up and the
treatment can be stopped. Prevention: There is no known way to prevent this
disorder.
Expectations
(prognosis)
Bullous
pemphigoid is a relatively benign disorder that tends to be chronic, with
flare-ups after long remissions. Infection of the skin lesions is the most
common complication. Although bullous pemphigoid can be a chronic condition, it
frequently undergoes spontaneous remission, much to the delight of both patient
and physician.
How do I take care of
blisters?
Supplies
needed? Ointment: Antibiotic ointment is a topical antibiotic available here.
Band-Aids or hypoallergenic paper
tape.
Gauze: Cotton gauze or cotton balls.
Saline: Available at your pharmacy.
Brief
routine Twice a day: Pour Saline onto the wound
or blister.
Twice a day: Lightly rub the area with
a Saline soaked gauze.
Twice a day: After the Saline,
liberally apply antibiotic ointment with a Q tip.
Twice a day: If you desire, you may
cover with a new bandage.
It's best to keep the wound
continuously moist with Antibiotic Ointment.
Severe wounds should not be exposed to
excessive water.
¼ While showering, a thick film of
antibiotic ointment will prevent water exposure.
½ Prevent
infection by keeping your fingers off the wound. Please avoid picking.
|
|
 |
|
|
 |
 |
|||||||||||
 |
|||||||||||||
Home | Dry/Sensitive Skin | Skin Renewal | Skin Complexion & Acne | Dermatology Patient Education |