Randy Jacobs, M.D. Patient Education
To return to the Patient Education page and read more articles, click here.

Exanthems - Rubella
CHILDHOOD
EXANTHEMS: Rubella
Introduction
Exanthems are a common cause of generalized
rashes in children. They pose a diagnostic challenge to even the most
experienced physician because of the diversity of their clinical presentations.
The morphology distribution, and associated signs and symptoms are sometimes
specific enough for a definitive diagnosis, but, nonspecific clinical findings
often make this impossible. Advances in laboratory techniques (particularly in
viral diseases), new antiviral drugs and vaccines, epidemics of old exanthems, and the recognition of new clinical syndromes
have stimulated renewed interest in exanthems.
Historically, exanthems were numbered in the order in
which they were first differentiated from other exanthems.
Thus, "first" disease was measles (rubeola),
"second" disease was scarlet fever, and "third" disease was
rubella (German measles). The specific disease described as "fourth"
disease, so-called Pilatov-Dukes disease, is no
longer accepted as a distinct clinical entity, with some authors speculating
that it represented staphylococcal scalded skin syndrome, and others
speculating that it was concurrent infection with both scarlet fever and
rubella. Fifth disease is erythema infectiosum, and
sixth disease is roseola infantum.
Only in the last decade, with the identification of parvovirus B19 as the cause
of erythema infectiosum and human herpesvirus 6 as the cause of roseola infantum,
have the causative agents of the classic exanthems been identified.
Rubella
Rubella
is also known as German Measles or Three-Day
Measles. Rubella is a contagious viral
disease characterized by swelling of Iymph glands and
a rash. A pregnant woman infected with rubella during the early months of
pregnancy may develop an abortion, stillbirth or congenital defects in the
infant.
Symptoms
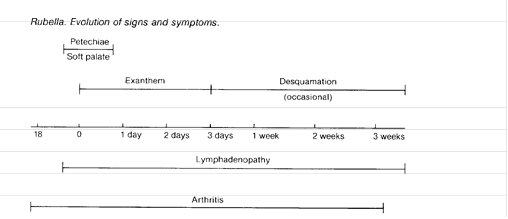
Rubella
has a 14- to 21-day incubation period and a 1- to 5-day preliminary phase in
children. The preliminary phase may be minimal or absent in adolescents and
adults. Tender swelling of the glands in the back of the head, the neck and
behind the ears is characteristic. The typical rash appears days after onset of
these symptoms. The rubella rash is similar to that of measles, but it is
usually less extensive and disappears more quickly. It begins on the face and
neck and quickly spreads to the trunk and the extremities. At the onset of the
eruption, a flush similar to that of scarlet fever may appear, particularly on
the face. The rash usually lasts about three days. It may disappear before this
time, and rarely there is no rash at all. A slight
fever usually occurs with the rash. Other symptoms such as headache, loss of
appetite, sore throat and general malaise, are more common in adults and
teenagers than in children. After-effects of rubella are rare among children,
although there have been cases of joint pain (arthralgia), sleeping sickness
and blood clotting problems. Adult women who contract rubella are often left
with chronic joint pains. Encephalitis is a rare complication that has occurred
during extensive outbreaks of rubella among young adults serving in the armed
services. Transient pain in the testes is also a frequent complaint in adult
males with rubella.
Cause
Rubella
is caused by an RNA virus of uncertain classification (probably a toga-virus),
and is spread by airborne droplet clusters or by close contact with an infected
person. A patient can transmit the disease from 1 week before onset of the rash
until 1 week after it fades. Congenitally infected infants are potentially
infectious for a few months after birth. Rubella is apparently less contagious
than measles, and many persons are not infected during childhood. As a result,
10% to 15% of young adult women are susceptible if they have not been
vaccinated against the disorder. Many cases are misdiagnosed or go unnoticed.
Before the rubella vaccine was developed, epidemics occurred at regular
intervals during the spring. Major epidemics occur at about 6 to 9 year
intervals. Once infected by rubella, immunity appears to be lifelong.
Similar Disorders
Measles,
scarlet fever (scarlatina), secondary syphilis, drug
rashes, erythema infectiosum (fifth disease),
infectious mononucleosis, and echo-, coxsackie- and
adenovirus infections must be considered in the differential diagnosis. Rubella
is clinically differentiated from measles by the milder rash that disappears
faster, and by the absence of the small, irregular, bright red spots (Koplik's spots) on the mucous membranes inside of the
cheeks and on the tongue, a running nose (coryza),
the aversion to light, and a cough. A patient with measles appears more sick, and the illness lasts longer. With even mild
scarlet fever (scarlatina), there are usually more
constitutional symptoms than in rubella, including a severely red, sore throat.
The white blood cell count is elevated in scarlet fever, but is usually normal
in rubella. The rash and swollen Iymph nodes (adenopathy) of rubella can be simulated by secondary
syphilis. However, the Iymph nodes are not tender in
syphilis and the rash appears bronze-like. If there is doubt, a quantitative
serologic test for syphilis can be performed. Infectious mononucleosis may also
cause a rubella-like swelling of Iymph nodes and a
skin rash, but can be differentiated by the initial lack of white blood cells
(leukopenia) followed by an increase in white blood cells (leukocytosis). Many
typical mononuclear cells appear in the blood smear, with appearance of
antibodies to the Epstein-Barr virus. In addition, the sore throat of
infectious mononucleosis is usually prominent, and malaise is greater and lasts
much longer than in rubella. A clinical diagnosis of rubella is subject to
error without laboratory confirmation, especially since many viral rashes
closely mimic rubella. Acute and convalescent serum should be obtained, if
possible, for serologic testing. A 4-fold or greater rise in specific hemagglutination inhibiting antibodies confirms the
diagnosis of rubella.
Therapy
Standard Therapies: Prevention is the most important
therapy. The purpose of rubella immunization programs is to prevent some of the
catastrophes associated with congenital rubella. All children between the ages
of 15 months and puberty should be routinely vaccinated against rubella. Women
of childbearing age whose blood tests negative for rubella hemagglutination inhibiting antibodies should be immunized. Conception should be prevented for
at least 3 months after immunization. Rubella, itself, requires little or no
treatment. Middle ear infection (otitis media), a rare complication, is usually
treated with penicillin or other antibiotic.
|
|