Randy Jacobs, M.D. Patient Education
To return to the Patient Education page and read more articles, click here.

Exfoliative Dermatitis
Exfoliative
dermatitis, also known as exfoliative erythroderma, begins as a rapidly
developing, generalized redness of the skin surface. Fine scales or thick
sheets of desquamation follow the erythrodermic stage. Pruritus (itching) may
be severe. Hair loss and nail abnormalities may accompany exfoliation.
Widespread lymph node enlargement, hepatosplenomegaly, and low-grade fever are
common. Because heat is radiated away from the erythematous (vasodilated) skin
surface, chills are typical, and life-threatening hypothermia may follow. The
diversion of substantial blood flow to the skin may result in cardiac failure.
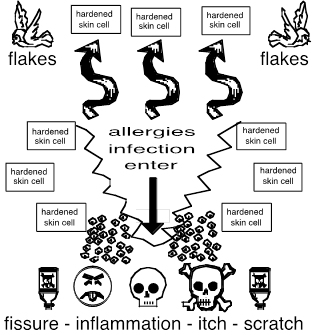
The loss of a normal epidermal skin barrier may lead to septicemia, and the
usual degree of debility that accompanies this disease predisposes the patient
to pneumonia and other infections.
What causes it?
You
can view exfoliative dermatitis as the end stage result of chronic inflammatory
skin disease and a completely damaged skin barrier. Exfoliative dermatitis is
usually caused by preexisting skin disease, especially psoriasis, atopic
dermatitis, severe seborrheic dermatitis, drug hypersensitivity to a variety of
antibiotics, anticonvulsants, and anti-inflammatory agents, and underlying
leukemia, lymphoma, or visceral malignancy. In some cases, a skin biopsy may be
helpful to define or confirm a preexisting dermatologic disorder or underlying
lymphoma, and therefore may be undertaken in all cases of unknown or uncertain
cause. Although the cause of the exfoliation may not be found, it often times
is found. Clues indicative of specific diseases may be found under close
scrutiny, such as the nail pitting of psoriasis, or the localization of atopic
dermatitis. A general medical workup is warranted, to help to determine the
presence of possible underlying malignancy or infection, and the extent of any
resultant metabolic derangement. A thorough history may reveal the use of a
causative drug, such as penicillin, sulfa, isoniazid, phenytoin, or
phenothiazines. Biopsy of involved skin may be performed, but may only yield
nonspecific findings.
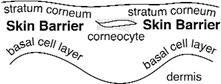
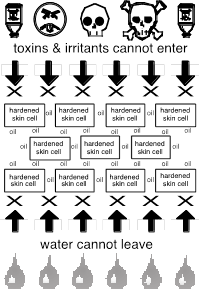
The human skin barrier is located in the uppermost skin
layer called the stratum corneum and has two primary physiological/physical
barrier functions:
1. An Exit Barrier: The skin barrier maintains skin
moisturization by preventing vital skin water from exiting the body i.e.
evaporation of water away into the air.
2. An Entrance Barrier: The skin
barrier minimizes skin inflammation, microbial, and other foreign contaminants
by preventing entrance of potential toxins, infectants, and allergens.
A Damaged Skin Barrier Is Evident.
Exfoliative
dermatitis is a rather rare erythematous scaling skin eruption which involves
all or nearly all of the cutaneous surface. The
condition may be a manifestation of any of a variety of underlying skin
diseases. In patients under the age of forty, it may be due to atopic
dermatitis, seborrheic dermatitis, staphylococcal scalded skin syndrome, or a
hereditary icthyosis. The eruption evolves rapidly if it is due to allergy,
lymphoma or leukemia (particularly in patients over forty), staphylococcal
infection, or contact allergens; it has a more gradual onset if there is a
primary skin disease which has spread, such as atopic dermatitis or psoriasis.
Often the etiologic diagnosis cannot be determined. Varying degrees of erythema
and scaling are seen which can range from fine, granular, generalized scales to
large, erythematous, lichenified plaques. Generalized lymphadenopathy may be
seen, as well as hair and nail involvement which frequently leads to the loss
of both. Itching tends to be generalized and extreme, and metabolic problems
may result from disruption of the barrier function of and increased blood flow
to the skin. Much water and heat may be lost through the affected skin, which
may result in dehydration, weakness, chills and fever, and hypothermia. There
may be considerable protein loss.
What Does The Skin Barrier Do?
The skin
barrier is a special skin structure that keeps vital fluids inside your body,
and prevents unwanted toxins, infections, and allergens from entering. The skin
barrier covers the entire body: You stay moisturized, free of inflammation, and
free of infection.
Therapy
Patients with
exfoliative dermatitis may need hospitalization. A high protein diet should be
initiated, because of the high degree of protein loss and high metabolic rate.
A high protein diet will help offset the negative nitrogen balance induced by
shedding layers of skin. Optimum skin care generally consists of continuous
application of tap water wet dressings followed by continuous applications of
an intermediate strength corticosteroid such as 0.1% triamcinolone ointment.
Dressings can be made from either terry cloth towels or heavy mesh gauze and
are to be changed and reapplied at 2 to 3 hour intervals. With clinical
improvement, the dressings may be changed less frequently, provided that
emollients are used also to help prevent dehydration of the skin between
dressing changes. Aveeno baths can take the place of these tap water wet
dressings. A lukewarm bath, perhaps with Aveeno added to the water to help
soothe itching, can be very helpful and is recommended one or more times daily
between dressing changes. Avoid allergic items in patients with exfoliative
dermatitis. Exfoliative dermatitis involved skin can become itchy when exposed
to allergic type substances such as perfumes, dyes, conditioners, powders,
anti-perspirants, hair sprays, grasses, plants, fragranced products, shampoos,
unrinsed laundry detergents, fabric softener sheets, dog or cat hairs, carpets,
chemicals, Aloe Vera, PABA, detergents, acrylic nails, polishes, nickel, elastic,
latex, etc. Hair conditioners can also induce itch! Please avoid all types of
perfume on the patient and on people in close proximity.
Persons with
exfoliative dermatitis involved skin may bathe or shower twice daily: 1. Use no
soap on dry or sensitive skin areas. You may use mild Gentle Face and Body
Cleanser, instead of soap. 2. After bathing, thoroughly lubricate your skin
using Cream available OTC. 3. After your bath, you should not towel dry. Wipe
off the water with your hands, then, apply a thick film of Cream to your entire
body. This film will seal in your new moisture. 4. For shampoo, use OTC fragrance free Gentle Shampoo. Mild lubricants, or anti-
pruritic creams, or mild hydrocortisone creams may be used all over the body to
soothe the inflammation. Oral antihistamines may be used to reduce itching.
Systemic
steroids may be helpful, but not in every case, as they may aggravate psoriasis
or Staphylococcal Scalded Skin Syndrome. Systemic antibiotics should be started
in any case as a broken skin barrier opens the door to infections such as staph
and strep. Antihistamines may be helpful in relieving pruritus (itching) and
providing needed sedation. With improvement in the skin condition, the patient
may be weaned off the steroids, antibiotics, and Aveeno baths. Gradually and
eventually they may be discontinued, but only under the guidance of a
physician.
Most cases of exfoliative erythroderma represent an
underlying skin barrier condition that has not been cared for properly, or has
gone out of control. After the exfoliative dermatitis is resolved, the patient
must be careful to again follow appropriate care for the particular underlying
condition whether it is atopic dermatitis, psoriasis, or simple chronic eczema.
ABC moisturization is of the utmost importance as taught in the ABC booklet
(you can download the ABC booklet off of our website). I suggest that you also
read the “Skin Barrier Education” sheet also available on our website.
|