Randy Jacobs, M.D. Patient Education
To return to the Patient Education page and read more articles, click here.

Acne: A Medical Point of Review
Ringworm (Tinea) General Patient
Education
Introduction
Ringworm
is a fungal (dermatophyte) infection of the skin, hair, or nails. It gets its
name from its appearance on the skin. There are two main varieties of fungi
causing dermatophyte infections: Trichophyton and Microsporum. Ringworm often
looks like a ring-shaped rash. Ringworm is caused by several different types of
fungi (molds). Other names for ringworm include tinea, dermatophytosis,
athlete's foot (ringworm of the feet), and jock itch (ringworm of the groin).
Ringworm cases have been given different medical names to describe the
locations of the fungal infection. Thus, tinea of the groin is call tinea
cruris after the Latin word for groin. Tinea of the scalp is called tinea
capitis after scalp. Tinea of the body is called tinea corporis. Tinea of the
feet is called tinea pedis. Tinea of the face is called tinea facei, and so on.
Do you get the nomenclature? It is not caused by a worm! You can get ringworm
from people, animals, or places. People get it through contact with a person
who has ringworm, or by using items such as clothes, towels, or hairbrushes
that were used by someone with a ringworm infection. Animals can carry some
types of fungi on their fur or skin without showing signs of ringworm
infection. Sick or carrier animals can transmit fungi to people by direct or
indirect (hair or dander) contact. Places like gyms, shower stalls, and floors
can transmit fungus if used by someone with ringworm. Other people can catch
the fungus if exposed to these places.
Ringworm
is easily diagnosed. A doctor can do some simple tests to determine whether a
rash is caused by a fungus. Ringworm is usually diagnosed by simple physical
examination. Ringworm can show classic physical exam findings such as the
erythematous scaled annular ring of the body or groin in tinea cruris, the dry
fine scale covering the soles of the feet like a "moccasin shoe" in
tinea rubrum, or the interdigital maceration and scaling found between the toes
in athlete's feet. Interestingly, there is a classic fungal presentation called
"two foot one hand disease" in which one hand and both feet are
involved with fungus. Why both hands are not involved is a medical mystery.
Treatment is usually an antifungal cream applied to the sites of infection, or
pills taken by mouth. If you have ringworm, you can avoid spreading it to
others by: Following Dr. Jacobs' advice for proper treatment: Keep your skin,
hair, and nails clean and dry. Wash towels and clothing in hot water and soap
to destroy the fungus. Stay away from common areas such as community pools and
gyms until your infection goes away. Ringworm can be prevented by: Keeping
common-use areas clean with bleach or Ajax cleanser. Using a floor and bath
cleaner that contains a fungus-killing "fungicidal" agent. Avoid
sharing clothing, towels, hair brushes, or other personal items.
![]() Tinea
Capitis and Barbae (Fungal Infections
of the Scalp and Face)
Tinea
Capitis and Barbae (Fungal Infections
of the Scalp and Face)
Tinea
capitis is a fungal infection of the scalp. It consist of cutaneous lesions caused by various species of dermatophytes: Trichophyton
and Microsporum. When the infection involves a man's beard, it is called Tinea
barbae. Tinea barbae is rare, and most skin infections of the beard area are
caused by bacteria, not fungus. Tinea capitis mainly affects children. Rarely,
an adult can develop Tinea capitis. It is a contagious infection and may become
an epidemic, being spread from child to child via hats or via the barber.
Occasionally, children acquire the infection from cattle or domestic animals
(dogs, cats). Tinea capitis infections can be grouped into four types based on presentation. The "black dot" type, the most
common in the U. S., is usually caused by Trichophyton tonsurans. It is subtle
in onset and characteristics. The inflammation is low-grade and persistent, the lesions are not annular or sharply
marginated. Affected areas of the scalp show characteristic black dots
resulting from broken hairs. The "gray patch" type is usually caused
by the Microsporum species, Microsporum audouini or Microsporum canis. M.
audouini lesions are small, scaly, semi-bald, grayish patches with broken
lusterless hair. The infection may be limited to a small area or may extend and
coalesce until the entire scalp is involved, sometimes with ringed patches extending
beyond the scalp margin. M. canis usually causes a more severe inflammatory
reaction with shedding of the infected hairs. The "kerion" type
presents with the development of a raised, inflamed, boggy granuloma and is
caused by Trichophyton verrucosum. It is seen, commonly, in children who have
been in contact with cattle or other domestic animals. There is dramatic, acute
folliculitis with pustules and swelling forming a boggy mass on the scalp. Hair
loss and eventual scarring alopecia are common, but one attack usually confers
subsequent immunity. Finally, the "favus (honeycomb)" type is due to
infection with Trichophyton schoenleini. The characteristic features include
extensive, even complete hair loss, scalp atrophy, and scarring leading to
permanent alopecia, and the presence of yellowish, adherent scales or crusts
(scutula) on the remaining hairs and scalp.
The
diagnosis may be made by presentation and examination of the scalp by physical
examination, biopsy with special stains, fungal culture, or with filtered
ultraviolet light (Wood's light). Tinea capitis caused by Microsporum species
reveals bright green hair shafts. The Trichophyton species do not reveal much
fluorescence, although T. schoenleini, the cause of the "favus" type,
causes a dull green fluorescence.
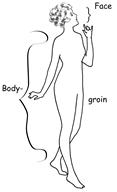
Tinea Corporis and Tinea Cruris (Fungal Infections: Body & Groin)
Tinea
corporis and tinea cruris are fungal infections of the body & groin. They
consist of cutaneous lesions caused by dermatophytes, a kind of skin fungi.
When the infection involves the upper thighs or groin, it is called tinea
cruris, commonly known as "jock itch". Tinea corporis can occur in
people of all ages. Occasionally, people acquire the infection from cattle or
domestic animals (dogs, cats). The infection can be acquired from animal
contact, human contact, or rarely, from the soil. The infection usually occurs
on the trunk, limbs, or face (facei), and often in other areas of exposed skin
such as the arms or neck. Tinea corporis and tinea cruris can occur anywhere.
The infections can also begin in the body folds such as the groin or armpits
and may present as an itchy, scaly, red area with a raised, spreading edge with
central clearing. The buttocks are a common location for tinea. These plaques
may consist of pustules or vesicles. As already stated, when it occurs in the
upper thighs or groin, it is called Tinea cruris or "jock itch".
Tinea cruris can be aggravated by tight clothing, obesity, and warm climates.
Humidity tends to favor growth of fungal organisms.
 Tinea Manus
and Onychomycosis (Fungal Infection:
Hands & Nails)
Tinea Manus
and Onychomycosis (Fungal Infection:
Hands & Nails)
Tinea
Manus is a chronic fungal infection of the hands. It consists of cutaneous
lesions caused by dermatophytes, usually Trichophyton rubrum. This fungus
inhabits nonviable tissue like the outer layers of the skin and nails and
generally does not invade living tissue. Tinea Manus is almost always
associated with a pre-existing Tinea Pedis, or fungal infection of the feet. It
is often on one hand only, and can involve the fingernails (Tinea Unguium).
When unilateral with tinea pedis, the condition is called Two Foot One Hand
Disease. One of the hardest to treat forms of external infection,
onychomycosis, aggressively discolors, thickens, and destroys the nail plate.
An estimated 10 million individuals in the continental United States suffer
from onychomycosis. People who work with their hands or on their feet, or those
who are frequently exposed to detergents, perspiration, and water, are at
higher risk for contacting onychomycosis. Nail fungal infections are prevalent
among the elderly, athletes, military personnel, and laborers, and may be more
severe in immunocompromised patients, particularly those with HIV.
What Does It Look Like?
In
tinea manus, the skin lesions usually consists of red , flaky, scaling hyperkeratotic patches or vesicles in clusters. The condition is
usually located on the palms or the dorsum and sides of the fingers. The
infection often involves or spreads to the toe and fingernails (Onychomycosis)
causing them to become thickened and lusterless. The nail plate can become
thickened, separated, and destroyed. Usually the infection and skin lesions
take months to clear and nail involvement may take up to a year. Quite often,
the nails never clear. Occasionally, the Tinea Manus will be caused by a fungus
that is resistant to griseofulvin.
 Majocchi's
Granuloma
Majocchi's
Granuloma
Most dermatophyte infections are superficial, but
Majocchi's granuloma is a dermatophyte infection that goes a bit deeper than
usual. Majocchi's granuloma (nodular granulomatous perifolliculitis) is a
well-recognized but uncommon infection of dermal and subcutaneous tissue by
fungal organisms (dermatophytes) usually limited to the superficial epidermis.
Majocchi's granuloma appears as deeply set bumps associated with hair follicles
of the skin. Because Majocchi's granuloma is a relatively uncommon lesion, most
reports have included only a few cases, and the spectrum of disease, the
organisms that cause it, and the population in which it occurs have not been
well defined. The fungal organism usually associated with Majocchi's granuloma
is Trichophyton rubrum. However, other dermatophytes including Trichophyton
mentagrophytes (variety granulosum), Trichophyton violaceum, Microsporum
audouini, Microsporum gypseum, Microsporum ferrugineum, or Microsporum canis
may be the causative agent. Majocchi's granuloma occurs as a localized dermal
infection, usually in individuals who have had chronic dermatophytosis but are
otherwise healthy. The initiating factor is thought to be physical trauma that
leads either directly or indirectly to disruption of the follicle and to
passive introduction of the organism deep into the skin, together with keratin
and/or necrotic material into the dermis. Majocchi's granuloma requires oral
therapy for treatment. Topicals are not effective.
"Id
Reaction"
"Autosensitization
dermatitis," also known as "autoeczematization," also known as
the "Id Reaction" is the vesicular eruption sometimes seen in
patients with an intense inflammatory process such as active stasis dermatitis
or acute fungal infections of the feet. The vesicular eruption most often involves the sides of the fingers but
can involve the entire body. Some feel that the "Id Reaction" is an
allergic reaction to the fungi or some antigen formed during the inflammatory
process. The vesicular eruptions
disappear as the initiating inflammation disapates. The diagnosis of
autoeczematization should be made only it there is an acute inflammatory
process at a distant site, and the reaction disappears shortly after the acute
inflammatory process is controlled.
Autosensitization
dermatitis (autoeczematization) is medically defined as the dissemination of a
previously localized area of chronic dermatitis to distant areas of the
skin. Autosensitization dermatitis
generally appears as itchy grouped pruritic papules, papulovesicles, and
eczematous patches on various regions of the body. Autosensitization dermatitis
usually occurs suddenly, but may develop gradually in some cases. Autosensitization dermatitis is not an
extension of previously localized dermatitis, per se, as there are "skip
areas" of normal skin between the primary process and secondary
occurence. The exact cause of this
phenomenon is not known, but it may have a cell-mediated autoimmune mechanism.
Autosensitization
dermatitis may also occur as an allergic reaction to a fungal infection
elsewhere on the skin. This type of
autosensitization dermatitis is also known as a dermatophytid, or "id
reaction." Although well
documented, the "id reaction" is actually quite rare. The diagnostic criteria for a dermatophytid
includes a proven fungal skin infection, a subsequent distant dermatitis devoid
of fungal elements, and resolution of the distant eczematous reaction upon
treatment of the primary fungal infection with appropriate antifungal
agents. Again, the exact cause of this
sort of socalled "autosensitization" is not really known.
The
successful treatment of autosensitization dermatitis "id reaction" with either an
eczematous or fungal primary process lies in the treatment of the primary
process. Once the original site is
completely cleared through the use of appropriate topical (or systemic, in the
case of some types of fungal infections) medications, the distant affected
sites may usually be expected to clear as well. Concomitant treatment of the distant sites with topical steroids is
often also helpful. Twice daily soaks of
affected areas with Burow's solution, as well as Aveeno oatmeal baths for more
widespread reactions, may also be helpful to relieve itching. If, however, clearing of the distant lesions
does not occur once the primary skin lesions have been successfully treated,
then, the diagnosis of autoeczematization is cast in doubt and other causative
factors may be sought.
How are tinea
infections treated?
Treatment
of Tinea corporis can consist of topical antifungal creams or lotions or oral
medications. The mild cases usually resolve within several weeks and topical
treatment should be continued for at least 30 days after the lesions disappear.
If the infection is more severe or resistant to topical treatment, oral
medications may be indicated. For tinea cruris, non irritating topical creams
or lotions may be indicated. If there is no response, or if irritation from the
topical antifungals develops, oral medications can be used. Tinea cruris
lesions may become complicated by secondary bacterial or other yeast or fungal
infections, and recurrence is common. Treatment of tinea capitis and tinea
barbae usually consists of oral medications, usually Griseofulvin for 1 to 2
months, or until the infection has cleared. Topical antifungal creams or
lotions may be helpful in preventing spread of tinea capitis to other children.
Oral antibiotics may be needed to treat tinea barbae if secondary bacterial
infection is also present. Also, oral steroids may be needed if severe
disfiguring inflammation is present on the scalp or face. Onychomycosis usually
requires longer term therapy with oral medications. Sometimes, the risks of liver inflammation or drug interactions is not
worth the benefits, and Dr. Jacobs may suggest control with topical gels or
solutions.
|
A Word About Oral Medications: If your tinea is
severe, Dr. Jacobs may discuss with you the possibility of using oral
medications to treat your infection. There are three main oral medications used
in the treatment of tinea: Griseofulvin, Nizoral Tablets, Lamisil Tablets, and
Sporanox Capsules. As with any medical decision, one must always weigh risks
and benefits when deciding on choosing a particular form of therapy. The oral
medications do have possible side effects that you should be informed of. You
should not use alcohol with these medications. You should inform Dr. Jacobs if
you have any history of alcohol intake, liver disease, hepatitis, or any
chronic diseases. All oral antifungal medications are listed as able to cause
side effects involving allergies, death, changes in
blood count, kidneys, and skin. Please read the package inserts for details.
Your pharmacist can also give you an informational sheet for each drug in
question. Of note, Nizoral is known to cause liver toxicity and inflammation in
1 in 10,000 patients. This has been fatal in certain patients, even after
taking the medication for a short time. Lamisil Tablets, and Sporanox Capsules can cause the same, but the incidence is much less, and
these are considered safer medications for long term use. To a lesser degree,
Griseofulvin is also known to cause liver toxicity and inflammation.
Griseofulvin does have a cross reactivity in patients who are allergic to
penicillin. If the benefits outweigh the risks in your condition, you may want
to take an oral medication for your infection. Dr. Jacobs may order blood
tests, initially, or after two weeks, and then periodically for Nizoral
Tablets, Lamisil Tablets, and Sporanox Capsules. Dr. Jacobs may order blood
tests, initially, and then at monthly or six week intervals for patients
requiring Griseofulvin for longer than 3 weeks. If you have any further
questions, please ask Dr. Jacobs at your next appointment. He will be happy to
help you.
Photos
of Fungal Infections


