Randy Jacobs, M.D. Patient Education
To return to the Patient Education page and read more articles, click here.

Keratosis Pilaris
 Keratosis Pilaris
Keratosis Pilaris
Clinical
Presentation
Keratosis
pilaris is a common condition of children and young adults in which tiny
follicular papules form. Keratosis pilaris consists of small clustered, firm,
white papules approximately one millimeter in diameter. The papules are found
in hair follicle distribution and are most often found on the lateral upper
arms and anterior thighs. The buttocks is occasionally
involved. The presence of keratosis pilaris causes the skin to have sandpaper
like feeling. Occasionally, an inflammatory halo of lighter skin surrounds the
white papules. The lesions of keratosis pilaris are located at follicular
openings of hair follicles, and often can be scooped out with a fingernail or
dermal curette. When this is done a coiled hair is sometimes found within the
white semisolid material. The lesions are usually symptomless, though sometimes
mild itching is present.
What
Causes Keratosis Pilaris?
Keratosis pilaris tends to run in families. A father or
mother may pass keratosis pilaris on to the children. Quite often, people with
keratosis pilaris may also have asthma, hay fever, and/or allergies. In this
setting, keratosis pilaris is a manifestation of a skin condition known as
atopic dermatitis. Microscopically, keratosis pilaris is found to be a peculiar
thickening and piling up of the tiny skin cells surrounding hair follicles.
This thickening and piling up results in the little bumps you can see and feel.
Course
and Prognosis
In keratosis
pilaris, the individual papules may come and go over a matter of weeks. In
general, the overall course is chronic and one cannot expect a complete cure.
Keratosis pilaris may be controlled, but not cured.
Therapy
As keratosis
pilaris may be controlled, but not cured, there
is no good treatment for the cause of keratosis pilaris. Prolonged bathtub
soaks, followed by mild scrubbing with a Buff Puff sponge may remove the plugs,
but the lesions of keratosis pilaris may quickly reform. Lubricants and
moisturizers, especially those with lactic acid or glycolic acid, may soften
the dry skin, which accompanies keratosis pilaris. The application of peeling
agents such as Retin-A or Tazorac can be tried, but the irritation they cause
may be more troublesome than any mild benefit, which is obtained. Lactic acid,
glycolic acid, and Retin-A may work to normalize the tiny cells around the hair
follicles so that thickening and piling up does not occur. Cortisone
medications may limit inflammation and thus help with symptoms.
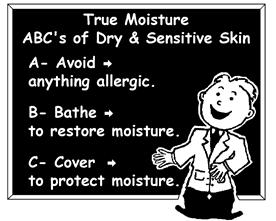 ABC Bathing: It
is important to avoid soap on areas of keratosis pilaris. Persons with
keratosis pilaris involved skin may bathe or shower twice daily: 1. Use no soap
on dry or sensitive skin areas. You may use mild Gentle Face and Body Cleanser,
instead of soap. 2. After bathing, thoroughly lubricate your skin using
Replenishing Cream available OTC. 3. After your bath, you should not towel dry.
Wipe off the water with your hands, then, apply a thin film of True Moisture®
Replenishing Cream to your entire body. This film will seal in your new
moisture. 4. For shampoo, use OTC fragrance free
Gentle Shampoo. Mild lubricants, or anti- pruritic creams, or mild
hydrocortisone creams may be used all over the body to soothe the inflammation.
Oral antihistamines may be used to reduce itching. Soap tends to dry the areas
and increases roughness. Finally, picking or extracting of lesions are not recommended as picking may result in secondary
infection with staph, strep, or other bacteria.
ABC Bathing: It
is important to avoid soap on areas of keratosis pilaris. Persons with
keratosis pilaris involved skin may bathe or shower twice daily: 1. Use no soap
on dry or sensitive skin areas. You may use mild Gentle Face and Body Cleanser,
instead of soap. 2. After bathing, thoroughly lubricate your skin using
Replenishing Cream available OTC. 3. After your bath, you should not towel dry.
Wipe off the water with your hands, then, apply a thin film of True Moisture®
Replenishing Cream to your entire body. This film will seal in your new
moisture. 4. For shampoo, use OTC fragrance free
Gentle Shampoo. Mild lubricants, or anti- pruritic creams, or mild
hydrocortisone creams may be used all over the body to soothe the inflammation.
Oral antihistamines may be used to reduce itching. Soap tends to dry the areas
and increases roughness. Finally, picking or extracting of lesions are not recommended as picking may result in secondary
infection with staph, strep, or other bacteria.

