Randy Jacobs, M.D. Patient Education
To return to the Patient Education page and read more articles, click here.

Melanoma
MOLES &
MALIGNANT MELANOMA
|
Introduction
There has been a
sharp increase in awareness of skin cancer in recent years as the result of a
worldwide campaign against this disease and reports about the thinning
atmospheric ozone layer, which is allowing greater penetration of harmful
ultraviolet rays. Skin cancer is the most common cancer. One in three cancers
diagnosed in the U.S.A. this year will be a skin cancer. One in six Americans
will develop skin cancer in his or her lifetime. In 1991, 600,000 new cases of
skin cancer were reported, and an estimated 8,500 deaths occurred from this
disease. Melanoma accounted for 6,500 deaths, while non-melanoma skin cancers
(basal cell carcinomas and squamous cell carcinomas) accounted for an estimated
2,000 deaths. Malignant melanoma is a skin cancer which occurs mostly in
adults, usually on the skin of the head, neck, legs, or back, and rarely in the
eye, mouth, vagina, or anus. Malignant melanoma may spread to other areas of
the body, primarily the lymph nodes, liver, lungs, and central nervous system.
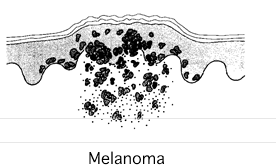
Most melanomas begin in a mole or other pre-existing skin lesion. They are flat
or slightly raised and can be black, brown, blue, red, white, or a mixture of
all colors. The borders are often irregular and may bleed. Melanoma is caused
by uncontrolled growth of cells that give skin its brownish color
(melanocytes). When the cells grow down into deep skin layers, they invade
blood vessels and lymph vessels and are spread to other body areas. This
process represents metastasis.
|
Risk of melanoma increases with:
- Moles on the
skin.
- Occupations or
activities involving excessive sun exposure, such as farming, construction
work, athletics, or sunbathing.
- Pregnancy.
- Genetic
factors. Melanoma is most common in people with light complexions. It is rare
in blacks.
- Radiation
treatment or excessive exposure to ultraviolet light, as with sun lamps or
tanning booths.
- A family
history of melanoma or a family history of dysplastic nevi.
Malignant Melanoma: Facts (Are the facts
related to a diminishing ozone layer?)
- In 1990 27,600 new cases of melanoma were
diagnosed; 14,800 occurred in males, 12,800 in females. An additional 5,000
cases of melanoma in-situ (early, non invasive lesions) were diagnosed.
- Approximately 50% of melanomas occur in
individuals younger than 55 years of age and approximately 30% occur in those
younger than age 45.
- The number of melanoma cases has nearly
doubled in the last decade, whereas the population has increased by only 11%.
- The incidence of malignant melanoma is
increasing at a rate faster than that of any other cancer. During the past
decade, the annual increase in melanoma was approximately 7% per year.
- In 1935, the lifetime risk of an individual
in the United States developing a malignant melanoma was 1:1500. In 1960, the
lifetime risk was 1:600; In 1980, the lifetime risk was 1:250; In 1990, the
lifetime risk was 1:105. It now is 1:75.
- For each decade since the 1940's, survival
rates have improved by approximately 10%. The 5-year survival rate for
malignant melanoma diagnosed between 1979-1984 was
80%. Statistics show that early diagnosis and prompt excision of the lesions
leads to cure in virtually all patients.
- Despite the increasing cure rate, the mortality
rate is also increasing because the disease incidence is increasing at an even
greater rate.
- Ten years ago, Melanoma was the 20th most
common cancer in the U.S. Melanoma is now the 8th most common cancer in the
U.S.
- A six fold increase in melanoma has occurred
in the U.S.A. in the last 50 years.
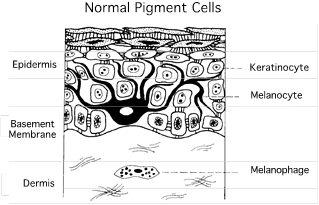
A. Definition
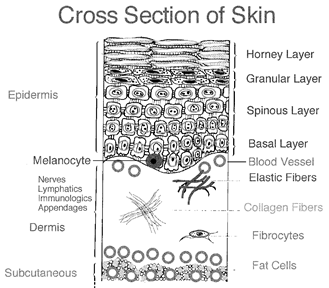
Melanoma is a
type of skin cancer involving the pigment producing cells of the skin (called
melanocytes, see adjacent diagram) The melanocyte
cells are responsible for the color of one's skin, as well as for the darkening
of skin seen after sun exposure. Melanocyte number is equal in all races.
B. The Four Forms of Melanoma
There are four major forms of melanoma, each is based
primarily on the type of growth pattern exhibited by the tumor. The most common
type of melanoma is called superficial
spreading melanoma, due to its rapid horizontal growth pattern. This kind
of melanoma is responsible for approximately 70% of all melanomas seen today. Nodular melanomas, which are
responsible for 15% to 30% of all melanomas, grow vertically into the dermis
and have a smaller radial component of growth. Nodular melanoma lesions are characterized by a cauliflower
 like appearance
which commonly arises without evidence of a pre-existing lesion. Nodular melanomas are blue to black in
color and may lack any pigment at all. These lesions are frequently more
aggressive and require immediate treatment. If pigment is absent, the melanoma
is called an amelanotic malignant melanoma. Amelanotic malignant melanomas are the most deceptive, as
they may closely resemble a variety of benign lesions. Lentigo maligna melanomas make up only 4% to 10
% of melanomas. They tend to be tan colored lesions that have been present for
numerous years as an enlarging dark spot on sun exposed skin. Lentigo maligna melanoma begins as a flat, irregularly bordered pigmented lesion called lentigo maligna. Lentigo maligna is
an in situ form of melanoma. This pigmented lesion may eventually evolve into
malignant melanoma. Because of its relation to malignant melanoma, Dr. Jacobs
is very aggressive in his treatment of Lentigo Maligna. The last major type of melanoma is acral lentiginous melanoma. Acral Lentiginous melanomas are responsible for only 2% to 8% of all melanomas, but are the cause
of up to 60% of melanomas in dark skinned people. They are flat brown and stain
like in nature with irregular borders. They are most commonly found on the
palms, soles or nail beds. Melanoma can begin in various ways. depending on the type of melanoma you are dealing with.
Superficial spreading melanoma tends to be found most commonly on the legs of
females and on the backs of men. This type is generally seen in fifth decade of
life. Nodular melanomas are seen more frequently in men and tend to grow fast
and have a palpable nodular component early on in the disease. Lentigo melanomas tend to take a long time to grow and are
commonly thought to be a freckle prior to diagnosis. They tend to be found on
the head and neck of those over 60 years of age. Acral lentiginous melanoma, as mentioned
before, are found on the palms, soles and nail beds. This type has both
vertical and horizontal growth components, however, may be merely a streak in
the nail with irregular tan brown staining of the nail bed. Moles are present
in about 1% of babies. Melanomas can often begin in larger congenital nevi. The larger the congenital
nevus, the larger the risk of acquiring melanoma. The risk of developing melanoma in a larger congenital nevus has been reported at 4.6 to 14%, depending on the
author. The size is the most important factor. The larger the
nevus, the greater the chance. The bottom line with large congenital
nevi is that they do have a chance
of converting to melanoma. Thus, the benefits may outweigh the risks when considering
removal of a large congenital mole. Small ones are less likely to convert. If
they appear atypical, these lesions can be removed at any time. It may be wise
to wait until a child is able to psychologicall understand the surgery. Ages 9 or 10 are usually appropriate. Dr. Jacobs may or
may not suggest removal. If a lesion is obviously atypical, Dr. Jacobs may
suggest removal at a younger age. Finally, other less common presentations of
melanoma include mucous membrane involvement such as the mouth, vagina, or
anus. In addition, certain giant hairy cell nevi or blue nevi can also lead to
melanoma. On occasion, melanoma can present in an organ, or metastatically without a demonstrable primary lesion. Lastly, certain families have members
with many moles which demonstrate features of the A,B,C,D's (see next page). Some call this condition the dysplastic or atypical nevus syndrome. Family members with this condition are at increased risk for
melanoma. If dysplastic nevi do exist in your family, you may want to discuss
this with Dr. Jacobs.
like appearance
which commonly arises without evidence of a pre-existing lesion. Nodular melanomas are blue to black in
color and may lack any pigment at all. These lesions are frequently more
aggressive and require immediate treatment. If pigment is absent, the melanoma
is called an amelanotic malignant melanoma. Amelanotic malignant melanomas are the most deceptive, as
they may closely resemble a variety of benign lesions. Lentigo maligna melanomas make up only 4% to 10
% of melanomas. They tend to be tan colored lesions that have been present for
numerous years as an enlarging dark spot on sun exposed skin. Lentigo maligna melanoma begins as a flat, irregularly bordered pigmented lesion called lentigo maligna. Lentigo maligna is
an in situ form of melanoma. This pigmented lesion may eventually evolve into
malignant melanoma. Because of its relation to malignant melanoma, Dr. Jacobs
is very aggressive in his treatment of Lentigo Maligna. The last major type of melanoma is acral lentiginous melanoma. Acral Lentiginous melanomas are responsible for only 2% to 8% of all melanomas, but are the cause
of up to 60% of melanomas in dark skinned people. They are flat brown and stain
like in nature with irregular borders. They are most commonly found on the
palms, soles or nail beds. Melanoma can begin in various ways. depending on the type of melanoma you are dealing with.
Superficial spreading melanoma tends to be found most commonly on the legs of
females and on the backs of men. This type is generally seen in fifth decade of
life. Nodular melanomas are seen more frequently in men and tend to grow fast
and have a palpable nodular component early on in the disease. Lentigo melanomas tend to take a long time to grow and are
commonly thought to be a freckle prior to diagnosis. They tend to be found on
the head and neck of those over 60 years of age. Acral lentiginous melanoma, as mentioned
before, are found on the palms, soles and nail beds. This type has both
vertical and horizontal growth components, however, may be merely a streak in
the nail with irregular tan brown staining of the nail bed. Moles are present
in about 1% of babies. Melanomas can often begin in larger congenital nevi. The larger the congenital
nevus, the larger the risk of acquiring melanoma. The risk of developing melanoma in a larger congenital nevus has been reported at 4.6 to 14%, depending on the
author. The size is the most important factor. The larger the
nevus, the greater the chance. The bottom line with large congenital
nevi is that they do have a chance
of converting to melanoma. Thus, the benefits may outweigh the risks when considering
removal of a large congenital mole. Small ones are less likely to convert. If
they appear atypical, these lesions can be removed at any time. It may be wise
to wait until a child is able to psychologicall understand the surgery. Ages 9 or 10 are usually appropriate. Dr. Jacobs may or
may not suggest removal. If a lesion is obviously atypical, Dr. Jacobs may
suggest removal at a younger age. Finally, other less common presentations of
melanoma include mucous membrane involvement such as the mouth, vagina, or
anus. In addition, certain giant hairy cell nevi or blue nevi can also lead to
melanoma. On occasion, melanoma can present in an organ, or metastatically without a demonstrable primary lesion. Lastly, certain families have members
with many moles which demonstrate features of the A,B,C,D's (see next page). Some call this condition the dysplastic or atypical nevus syndrome. Family members with this condition are at increased risk for
melanoma. If dysplastic nevi do exist in your family, you may want to discuss
this with Dr. Jacobs.
C. What causes it?
 Evidence suggests
that the most common inducing cause of melanoma is sun exposure. Hereditary
forms of melanoma may arise from moles and any suspicious lesions. A dose of
sun may be the factor that turns a normal mole into a melanoma. Melanomas
arising from congenital moles may undergo malignant transformation after some
kind of irritating exposure. Patients with fair complexions, red hair, blue
eyes, and those who tend to burn easily in the sun are at a particularly high
risk. Other risk factors include those who have received a transplant, or
patients with leukemia, lymphoma, or other immunosuppression.
Evidence suggests
that the most common inducing cause of melanoma is sun exposure. Hereditary
forms of melanoma may arise from moles and any suspicious lesions. A dose of
sun may be the factor that turns a normal mole into a melanoma. Melanomas
arising from congenital moles may undergo malignant transformation after some
kind of irritating exposure. Patients with fair complexions, red hair, blue
eyes, and those who tend to burn easily in the sun are at a particularly high
risk. Other risk factors include those who have received a transplant, or
patients with leukemia, lymphoma, or other immunosuppression.
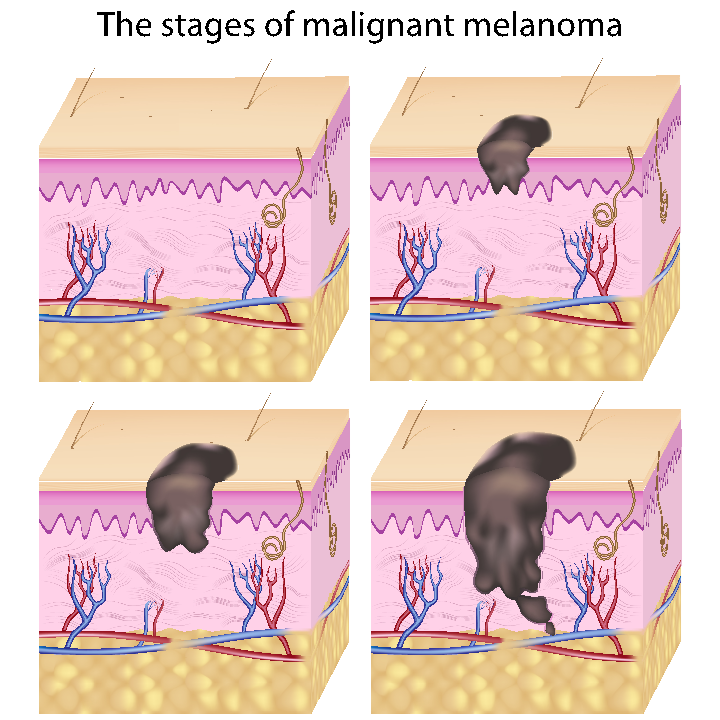
D. How does it progress?
The expected
outcome varies greatly. Early melanomas that have not grown far downward are
often curable by surgical removal. Once the tumor has spread to distant organs,
the condition may be incurable. Scientific research into causes and treatment, continues, so there is hope for increasingly
effective treatment and cure. The progression of the disease depends largely on
the type of melanoma you may have. Some types may progress very rapidly, such
as the nodular type, where others such as the lentigo maligna type melanomas make take years to progress.
Metastatic potential and lethality of the disease depends mostly on the depth
of invasion. Metastasis is possible with all types of malignant melanoma
tumors. For melanoma, an ounce of prevention is worth a pound of cure. The
patient with a history of melanoma should be followed closely for any signs of
recurrence. Dr. Jacobs likes to include a total body skin exam at regular
intervals throughout the year.
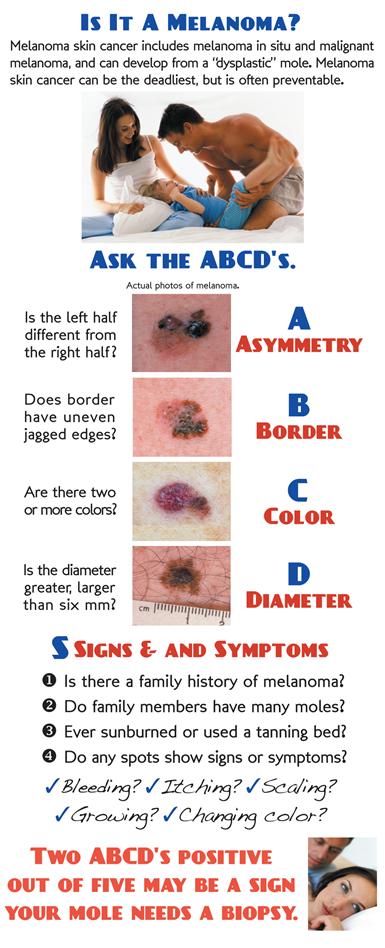
E. How is it diagnosed?
 Diagnosis is
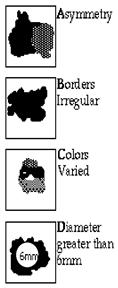
first obtained by a clinical evaluation of the lesion. Suspicious lesions contain
at least 2 of the 5 ABCD's of melanoma (see adjacent diagram). The S stands for signs, symptoms, and
significant factors (SSS) such as
itch, bleeding, enlargement, color change, and a family history of many moles
or melanoma. Dr. Jacobs suggests that any lesion with at least 2 of the 5 criteria should be biopsied and sent out for a pathological
diagnosis.
Diagnosis is
first obtained by a clinical evaluation of the lesion. Suspicious lesions contain
at least 2 of the 5 ABCD's of melanoma (see adjacent diagram). The S stands for signs, symptoms, and
significant factors (SSS) such as
itch, bleeding, enlargement, color change, and a family history of many moles
or melanoma. Dr. Jacobs suggests that any lesion with at least 2 of the 5 criteria should be biopsied and sent out for a pathological
diagnosis.
F. Ways to treat it.
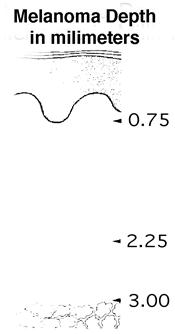 Surgical excision
is the most common and longest lasting procedure used to treat melanoma.
Surgery, however, is used only on accessible lesions and can be limited by the
patient's health and ability to undergo such a procedure. The extent of surgery
depends on the depth of invasion. Most authors recommend a wide surgical
excision for melanomas. In general, for lesions of the head and neck area, less
than 1.0 mm in thickness, a 1 cm margin appears to be
adequate. For those of 1-2 mm in thickness, a 2 cm margin. For those more than 2.0 mm in thickness, a 3 cm margin
is the maximum used. If lymph nodes are involved, the surgery may
be rather complex and not indicated some cases. In general, an elective lymph
node dissection (ELND) will be offered for patients with tumors between 1.5 and
4.0 mm in thickness. Radiation therapy is used primarily as a method of
relieving pain from distant metastatic sites. It may be used to control
superficial metastasis in the skin or soft tissues, as well. Chemotherapy is used, however, response rates are frequently poor and short
lived. Immunotherapy using newer drugs has in some cases been used with limited
success, but at this period of time, most immunotherapy is only experimental
and not completely effective. Bacillus Calmette-Guerin
(BCG) is a non specific immunostimulant which
increases the body's own immune reaction to melanoma. BCG may be used in
combination with DTIC (Dimethyl triazeno imidazole carboxamide), a chemotherapeutic agent for chemoimmunotherapy. Melanoma tumor vaccines are under
investigation, but have not as yet gained FDA approval. Biologic response
modifiers such as interleukin 2 and interferon may be used in certain cases,
but the side effects are difficult to endure. Other immunomodulating therapies include
monoclonal antibody therapy (injection of antibodies) and adoptive
immunotherapy. Adoptive immunotherapeutic methods involve removing, growing,
and concentrating the patient's own white blood cells, and reinjecting them. Though immunotherapy is primarily experimental at this time, we expect to
have fully functional immunotherapeutic treatment modalities in the next
several years. Special case: Pregnancy. Several studies suggest that pregnancy
has an adverse effect on melanoma. Dr. Jacobs suggests total skin exams for
pregnant patients at risk for melanoma. Melanoma in a pregnant patient should
be treated promptly and adequately in a manner that does not compromise the
patient's chances for cure.
Surgical excision
is the most common and longest lasting procedure used to treat melanoma.
Surgery, however, is used only on accessible lesions and can be limited by the
patient's health and ability to undergo such a procedure. The extent of surgery
depends on the depth of invasion. Most authors recommend a wide surgical
excision for melanomas. In general, for lesions of the head and neck area, less
than 1.0 mm in thickness, a 1 cm margin appears to be
adequate. For those of 1-2 mm in thickness, a 2 cm margin. For those more than 2.0 mm in thickness, a 3 cm margin
is the maximum used. If lymph nodes are involved, the surgery may
be rather complex and not indicated some cases. In general, an elective lymph
node dissection (ELND) will be offered for patients with tumors between 1.5 and
4.0 mm in thickness. Radiation therapy is used primarily as a method of
relieving pain from distant metastatic sites. It may be used to control
superficial metastasis in the skin or soft tissues, as well. Chemotherapy is used, however, response rates are frequently poor and short
lived. Immunotherapy using newer drugs has in some cases been used with limited
success, but at this period of time, most immunotherapy is only experimental
and not completely effective. Bacillus Calmette-Guerin
(BCG) is a non specific immunostimulant which
increases the body's own immune reaction to melanoma. BCG may be used in
combination with DTIC (Dimethyl triazeno imidazole carboxamide), a chemotherapeutic agent for chemoimmunotherapy. Melanoma tumor vaccines are under
investigation, but have not as yet gained FDA approval. Biologic response
modifiers such as interleukin 2 and interferon may be used in certain cases,
but the side effects are difficult to endure. Other immunomodulating therapies include
monoclonal antibody therapy (injection of antibodies) and adoptive
immunotherapy. Adoptive immunotherapeutic methods involve removing, growing,
and concentrating the patient's own white blood cells, and reinjecting them. Though immunotherapy is primarily experimental at this time, we expect to
have fully functional immunotherapeutic treatment modalities in the next
several years. Special case: Pregnancy. Several studies suggest that pregnancy
has an adverse effect on melanoma. Dr. Jacobs suggests total skin exams for
pregnant patients at risk for melanoma. Melanoma in a pregnant patient should
be treated promptly and adequately in a manner that does not compromise the
patient's chances for cure.
G. What to expect.
The prognosis of
the disease is dependent upon the location, tumor thickness and type, gender,
ulceration, and site of the primary lesion. Those with lymphatic involvement
must also consider the number of nodes affected and the possibility of distant
metastasis. Lesions which are localized and up to 0.76 - 1.50 mm deep have a 87 - 94% five
year survival if treated by surgical excision. It is, therefore, essential that
any suspicious lesions be evaluated by Dr. Jacobs as soon as possible. The key
to survival is early detection. With melanoma, an ounce of prevention is worth
a pound of cure. A stitch in time can save nine. If you have had a melanoma,
there is an increased risk of developing a second melanoma. For this reason, most melanoma patients are
seen back in Dr. Jacobs' clinic for a total body skin exam at least every three
months during the first post operative year, every six months during the
second, and every year thereafter.
H. Sentinal Lymph Node Dissection (SLND)
When clinically undetectable
cancer cells from a primary melanoma have spread (metastasized) to the regional
lymph nodes, these microscopic cells are most likely to be found in the sentinel
node, the first node in the lymphatic drainage channel closest to the site of
the primary tumor. This node can be located (mapped) by injecting a vital blue
dye intradermally around the primary tumor, or around
the biopsy site if the primary was previously removed. The dye is taken up by
the surrounding lymphatics and drains into the
regional lymph node basin, accumulating in the first node. A small incision is
made over the basin, where this now blue-tinted sentinel node can be visually
detected. It is removed and examined by a pathologist, and if no melanoma cells
are found, surgery is terminated and all other nodes can be spared (unlike
ELND, which always entails radical removal of all nodes). If cancerous cells
are found in the sentinel node, surgery continues to remove the rest of the
nodes.
Dr. Morton of UCLA, in his
original 1992 study found that the sentinel node could be identified 80 percent
of the time and accurately reflected the presence or absence of disease in 95
percent of patients evaluated. Many physicians soon embraced this selective
surgical technique in lieu of ELND, hoping to avoid the high cost,
disfigurement, and potential complications of unnecessary extensive surgery.
All that remained was for other research to confirm Morton's findings.
SLND has rapidly made its way into clinical practice, due to its cost-saving, morbidity-sparing possibilities. It has been spurred further by FDA approval of interferon alfa-2b therapy for melanoma patients who are at high risk of recurrence after tumor surgery. Many surgeons are using SLND to search for regional microscopic metastases to determine whether patients should receive interferon treatment.
I.
INTERFERON
Interferons are natural substances produced by the normal cells of most body tissues in response to viral infections and disease. Manufactured forms of interferons have been shown to help the body's immune system fight disease more effectively. There are three general types of interferons that are used to treat human diseases, interferon alfa, interferon beta, and interferon gamma. To date only interferon alfa has been found to be useful in treating cancer.
The immune system enables the
body to distinguish cells that are native to the body from those cells and
sub-cellular organisims that are foreign. These
foreign invaders include viruses, bacteria, and other disease-causing
organisms. The body recognizes foreign, diseased, or cancerous cells by special
marker substances known as antigens on their surfaces. These markers allow your
body's immune system to distinguish abnormal or foreign cells from healthy
cells in the tissues of your body. When this occurs, the immune response sends
an array of immune cells to contain and destroy or wall off the foreign or
cancerous invading cells.
Cells of the body's immune
system that have been stimulated or recognized antigens against which they are
targeted will begin to produce interferons and other
natural immune signalling substances. These
substances not only combat foreign invaders, which may cause infection, they
can also prevent the growth and spread of other diseased cells, including
cancer.
One type of interferon,
interferon alfa-2b, has been shown in two randomized prospective trials to
prolong disease-free and overall survival in patients with high-risk melanoma.
These results led to the U.S. Food and Drug Administration approval of
interferon alfa-2b as adjuvant therapy for melanoma in 1996. In other studies,
high dose interferon produced promising results in terms of delaying relapse in
stage II patients, while little if any benefit was seen in high-risk patients.
Clinical trials are currently
underway to further evaluate whether the highly significant benefit of
high-dose interferon given for a full year can be duplicated with the treatment
given for only one month, or a new form of long-acting less toxic (PEG)
interferon given weekly for many years. Other promising approaches may include
melanoma vaccines or combinations of interferon with other forms of
immunotherapy, such as interleukin-2.
Interferon Administration
Interferon therapy cannot be
administered orally because strong acids and enzymes in our digestive systems
would destroy it. Therefore, interferon must be delivered directly into the
blood stream or into tissue. In the first phase of interferon therapy, called
the induction phase, interferon is administered to the patient intravenously.
This may be done in a hospital or in an office setting. The induction phase
generally involves five days of interferon therapy per week for a four-week
period. Each subcutaneous injection should take about twenty to thirty minutes.
The second phase of
interferon therapy, called the subcutaneous injection maintenance phase, begins
in the fifth week and involves three injections per week. This routine
continues for the remainder of the year. During this phase many patients and
their loved ones learn to administer the injections of interferon themselves.
Interferon Side Effects
As with any treatment, the
side effects of interferon therapy depend on the prescribed dose. In addition,
all people differ in their individual responses to therapy. Thus, some patients
will have many side effects, while others may have none at all. Often, patients
experience the most side effects during the first few weeks of therapy. After
this period, many patients find that their side effects diminish greatly. Many
patients tolerate low dose therapy very well, while high-dose interferon
therapy tends to produce more severe and consistent side effects.
The main side effects of
interferon therapy are fatigue and flu-like symptoms. Flu-like symptoms include
fever, chills, headache, and general body aches. Another common symptom is loss
of appetite. Diminished appetite can sometimes be attributed to feelings of nausea
or the development of a metallic taste in the mouth. Less common side effects
include mild hair thinning, dry itchy skin, palpitations, and lightheadedness.
If side effects are severe, you should inform your doctor about and ask about
all possible solutions.
Some laboratory tests may
become abnormal with high-dose interferon including blood counts (5%), liver
enzymes (14%) and kidney and thyroid function (> 10%). These side effects
are generally reversible when therapy is stopped. If the symptoms or signs are
significantly abnormal, the treatment may be interrupted for a time, and then
resumed at a lower dose. Throughout the course of the therapy, treatment may be
stopped and restarted at different dosages as needed.
J. Scar Abrasion and Cosmetic Appearance
After
skin cancer surgery, Dr. Jacobs may use a small sanding device to "sand
down" the scar, or may perform some other procedure to improve the site.
Again, this type of work is exceedingly uncommon, and most patients do very
well with just a simple surgical removal. Finally, with all surgical therapies
rendered, there is always a small chance of incomplete removal or recurrence.
Dr. Jacobs handles each case individually, based on the patient's tumor, the
location, the size, the patient's wishes, and overall health. Please understand
that skin cancer therapy is often more than on step. The patient may need one
or more sessions in order to remove the cancer. Also, the patient may need
additional cosmetic work to restore the appearance of the site. Time and
patience is needed to achieve the desired result. For example, if an eyebrow or
nose is stretched after surgery, a second procedure may be needed to restore
the appearance. If a scar is large, a second procedure may be needed to improve
its appearance. This all takes time and waiting as the human body takes time to
decrease swelling, stretch, and heal after surgery.
K. Preventative Measures
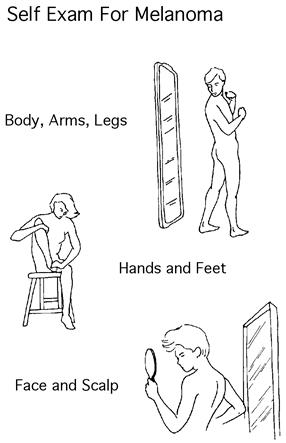
Early Detection and Diagnosis
It is important to detect melanoma as early as possible. A self-examination of the skin is also important to detect new growths or other changes. If you notice any changing, new, or odd-looking mole or skin change, contact Dr. Jacobs promptly. He will take a medical history and give you a physical examination.
Importance of early detection of melanoma
*Survival rates of patients
with thin primary melanomas are much higher than those for patients with thick
primary melanoma
*The probability of 10-year
survival for patients with melanomas less than 1 mm is about 95%
*The probability of 10-year
survival for patients with melanomas greater than 4 mm is less than 50%
*Recent improvements in
survival rates can be attributed to earlier detection
— Greater than 80% of
patients diagnosed in the 1990s are anticipated to survive long-term
If Dr. Jacobs thinks the mole
or skin change looks suspicious, a procedure known as a biopsy should be
performed. To perform a biopsy, Dr. Jacobs will inject a local anesthetic under
the skin to numb the area. The entire mole, or a piece of the mole, will be
removed and examined in a laboratory to determine if it is cancerous. In
general, superficial shave biopsies (slicing through the outer layers of the mole) are not recommended if melanoma
is suspected because the sample obtained may not take the complete melanoma,
and accurate measurement of the entire thickness of a melanoma is then not
possible. However, a deep shave biopsy is adequate. Therefore, Dr. Jacobs may
offer you a deep shave biopsy, a punch biopsy, or an excisional biopsy each of
which can go down deep enough to attain an adequate diagnosis. Protect yourself
from excessive sun exposure. Wear broad-brimmed hats and protective clothing.
Use maximum protection UVA & UVB sun block preparations on exposed skin.
Examine your skin, including soles of the feet, regularly for changes in
pigmented areas. Ask a family member to examine your back. See Dr. Jacobs about
any other skin areas (especially brown or black) that become multicolored,
develop irregular edges or surfaces, bleeds, or changes in any way. Use the space on the back of this page to
write down any findings from your own self exam. Please notify Dr. Jacobs if
there are any positive findings.
L. Photos
As
a picture is worth a thousand words, here are photos to help you understand
melanoma:

 \
\