Randy Jacobs, M.D. Patient Education
To return to the Patient Education page and read more articles, click here.

Psoriasis Education
PSORIASIS Q & A DEFINITION
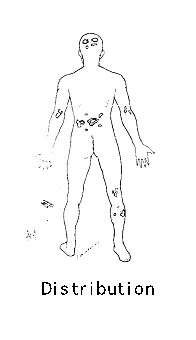 |
Psoriasis is a common, recurring skin condition in which the skin develops reddish silvery plaques and scales. Psoriasis most often affects the scalp, trunk, and outer sides of the arms and legs. Itching is common. The palms and soles may also be involved. The face is usually spared. Psoriasis is a persistent skin disease that got its name from the Greek word for "itch." The skin becomes inflamed, producing red, thickened areas with silvery scales, most often on the scalp, elbows, knees, and lower back. In some cases, psoriasis is so mild that people don't know they have it. At the opposite extreme, severe psoriasis may cover large areas of the body. Doctors can help even the most severe cases. Psoriasis cannot be passed from one person to another, though it is more likely to occur in people whose family members have it. In the United States two out of every hundred people have psoriasis (four to five million people). Approximately 150,000 new cases occur each year. How common is psoriasis? Current figures indicate that there are approximately eight million people in this country suffering from psoriasis. Psoriasis affects 1-2% of the population, or 1 in 20 people. Unfortunately, psoriasis is associated with Metabolic Syndrome, and patients with untreated psoriasis can have increased hypertension, diabetes, and up to a 4X risk of heart attack. Thus, if you have psoriasis, you should get treated! |
|
|
HOW IT BEGINS Psoriasis may begin as red itchy skin, a scaling scalp, or as scaly areas of the elbows and knees. Who gets psoriasis? About 60% of people with psoriasis have a family history of the disease. Men and women of all ages, all races, and all nationalities can get psoriasis. In other words, psoriasis can affect practically anyone. You can know you are not alone with your psoriasis. One third of patients are younger than 20 years at the time of onset, especially female patients. However psoriasis occurs equally in men and women. Silvery-white plaques may be scattered or generalized and vary in size. Beneath the plaques, the skin is red. Hair loss is not common, even if the scalp is involved. Finger and toenails often show changes in color with yellow-brown spots under the nail, and pitting. There may be a separation of the nail from the nail bed. Psoriasis may also be associated with arthritis, fever, weakness, chills, and pustules. Psoriasis can present as anything from a simple nuisance to a debilitating disease. |
WHAT CAUSES IT
The cause is unknown. However, recent discoveries point to an abnormality in the functioning of key white cells in the blood stream triggering inflammation in the skin. This causes the skin to shed itself too rapidly, every three to four days. People often notice new spots 10 to 14 days after the skin is cut, scratched, rubbed, or severely sunburned. Psoriasis can also be activated by infections, such as strep throat, and by certain medicines. Flare-ups sometimes occur in the winter, as a result of dry skin and lack of sunlight. The cause of psoriasis is unknown, but its particular pattern as it applies to you can be tracked by Dr. Jacobs. Though the cause is not known, treatment is available to help ease the symptoms. There is no "cure" for psoriasis, only control. Psoriasis is a hereditary disorder. If you have a parent affected by psoriasis you have a 10% chance of being affected. If both parents have psoriasis your chances increase to 30%. Psoriasis mainly occurs in Caucasians. The epidermis or outer layer of skin is constantly manufacturing new cells. Normally for skin cells to grow from the lower basal layer to the outermost skin surface requires 28 days. In psoriasis this process is tremendously rushed, and takes only 4 or 5 days. Instead of inconspicuously shedding, the outer skin cells pile up and form scales, which remain heaped up on the skin. People with psoriasis have certain areas of skin, which in which the skin cells grow much faster than usual. Those areas form patches of tough, scaly skin that may first appear as a red area of inflammation on knees, elbows and other joints, under the nails, and on the scalp. These are the lesions of psoriasis. A streptococcal sore throat in children may trigger an attack of psoriasis. This type of psoriasis is called "Guttate" and the lesions are round and small resembling drops of water sprinkled over the body. Adults with chronic psoriasis may also have a flare-up of psoriasis two weeks after a strep throat infection. Is psoriasis contagious? Despite its association with streptococcal sore throat, psoriasis is a benign skin condition, not an infection, and cannot be spread from person to person. Physical trauma such as scratching, though, can cause the disease to appear in different areas of the body of the same individual. 
HOW DOES IT PROGRESS?
Psoriasis comes in many forms. Each differs in how bad it is, how long it lasts, where it is, and in the shape and pattern of the scales. The most common form begins with little red bumps. Gradually these grow larger and scales form. While the top scales flake off easily and often, scales below the surface stick together. When they are removed, the tender, exposed skin bleeds. These small red areas then grow, sometimes becoming quite large. Elbows, knees, groin and genitals, arms, legs, scalp, and nails are the areas most commonly affected by psoriasis. It will often appear in the same place on both sides of the body. Nails with psoriasis have tiny pits on them. Nails may loosen, thicken or crumble and are difficult to treat. Inverse psoriasis occurs in the armpit, under the breast and in skin folds around the groin, buttocks, and genitals. Guttate psoriasis usually affects children and young adults. It often shows up after a sore throat, with many small, red, drop-like, scaly spots appearing on the skin. It often clears up by itself in weeks or a few months. About seven percent of psoriasis patients also have arthritis, which fortunately is not too severe in most people. In some people, the arthritis is worst when the skin is very involved. Sometimes the arthritis improves when the condition of the patient's skin improves. In general, the course of psoriasis is unpredictable and irregular. With treatment, the plaques will frequently disappear entirely or retreat to a few spots on the elbows or knees. These minimal spots, with some nail pitting, may remain for years. As patches get thicker and tougher, they may begin to flake off. If this happens on the scalp, the condition may be mistaken for dandruff. Under stress or for other unknown reasons the rash may often flare again. With treatment, there are often long periods of freedom from skin trouble. Patience is required. Minor trauma is a major factor in eliciting lesions. Scratching or rubbing should be avoided. Certain drugs systemic corticosteroids, lithium, alcohol, and chloroquine may make psoriasis worse. Excessive sunlight, stress, and body weight may exacerbate pre-existing psoriasis. Whenever it is possible, avoid situations of stress that may aggravate psoriasis. The more you worry, the worse you may get. Hot, humid environments tend to make bad cases of psoriasis worse. Sunny, dry climates can be helpful. Exposure to sunlight or artificial light should be done cautiously as a sunburn may do considerable harm. Severe sunburn may cause psoriasis to spread over the sunburned areas. Though sunlight helps psoriasis in the majority of patients, 10% of people may be made worse by any amount of sun. Sunscreen should be used consistently in these patients. Does psoriasis stay with you forever? It may or may not. Psoriasis doesn't appear with any regularity. It may appear, then disappear for a while, only to reappear again later. Some of the factors that can cause your psoriasis to flare up include bruises, cuts, scrapes, burns, prolonged irritation, certain drugs, bacterial and viral infections, long exposure to low humidity, stress, and anxiety.
HOW IS IT DIAGNOSED?
Dermatologists diagnose psoriasis by examining the skin, nails, and scalp. They may need to take a skin biopsy to examine under the microscope. The white-silvery scales of psoriasis are so distinctive that it is relatively easy to diagnose. Where the scales are not evident as often occurs in people who bathe and scrub frequently, scratching the lesions will show typical scales. Further scratching will show bleeding pinpoints, which are also characteristic of the disease. Nail changes occur in 25% of people with psoriasis. These characteristics plus the distribution of the lesions and family history lead to the diagnosis. In cases of doubt, a biopsy will provide confirmation. Seborrheic Dermatitis, fungal infections, drug reactions, and some systemic diseases may be difficult to differentiate without a biopsy. Especially in children, throat culture and blood tests may be needed for patients having the "Guttate" type of psoriasis. A psoriasis like eruption also occurs in Reiter's Syndrome.
WAYS TO TREAT PSORIASIS
 For the most part, treatment of psoriasis consists mainly of agents applied to the skin, not taken internally. The goal is to reduce inflammation and to slow down rapid skin cell division. Moisturizing creams and lotions loosen scales and help control itching. Special diets have not been successful in treating psoriasis. Treatment is based on a patient's health, age, lifestyle, and the severity of the psoriasis. Different types of treatments and several visits to Dr. Jacobs may be needed. The doctor may prescribe medications to apply on the skin containing cortisone-like compounds, synthetic vitamin D, tar, or anthralin. These may be used in combination with natural sunlight or ultraviolet light. The most severe forms of psoriasis may require oral medications, with or without light treatment. Sunlight exposure helps the majority of people with psoriasis but it must be used cautiously. Ultraviolet light therapy may be given in a dermatologist's office, a psoriasis center or a hospital. Types of Treatment: Steroids (Cortisone)--Cortisone creams, ointments, and lotions may clear the skin temporarily and control the condition in many patients. Weaker preparations should be used on more sensitive areas of the body such as the genitals, groin, and face. Stronger preparations will usually be needed to control lesions on the scalp, elbow, knees, palms and soles, and parts of the torso and may need to be applied under dressings. These must be used cautiously and with Dr. Jacobs' instructions. Side effects of the stronger cortisone preparations include thinning of the skin, dilated blood vessels, bruising, and skin color changes. Stopping these medications suddenly may result in a flare-up of the disease. After many months of treatment, the psoriasis may become resistant to the steroid preparations. Dr. Jacobs may inject cortisone in difficult-to-treat spots. These injections must be used in very small amounts to avoid side effects.
For the most part, treatment of psoriasis consists mainly of agents applied to the skin, not taken internally. The goal is to reduce inflammation and to slow down rapid skin cell division. Moisturizing creams and lotions loosen scales and help control itching. Special diets have not been successful in treating psoriasis. Treatment is based on a patient's health, age, lifestyle, and the severity of the psoriasis. Different types of treatments and several visits to Dr. Jacobs may be needed. The doctor may prescribe medications to apply on the skin containing cortisone-like compounds, synthetic vitamin D, tar, or anthralin. These may be used in combination with natural sunlight or ultraviolet light. The most severe forms of psoriasis may require oral medications, with or without light treatment. Sunlight exposure helps the majority of people with psoriasis but it must be used cautiously. Ultraviolet light therapy may be given in a dermatologist's office, a psoriasis center or a hospital. Types of Treatment: Steroids (Cortisone)--Cortisone creams, ointments, and lotions may clear the skin temporarily and control the condition in many patients. Weaker preparations should be used on more sensitive areas of the body such as the genitals, groin, and face. Stronger preparations will usually be needed to control lesions on the scalp, elbow, knees, palms and soles, and parts of the torso and may need to be applied under dressings. These must be used cautiously and with Dr. Jacobs' instructions. Side effects of the stronger cortisone preparations include thinning of the skin, dilated blood vessels, bruising, and skin color changes. Stopping these medications suddenly may result in a flare-up of the disease. After many months of treatment, the psoriasis may become resistant to the steroid preparations. Dr. Jacobs may inject cortisone in difficult-to-treat spots. These injections must be used in very small amounts to avoid side effects.
Scalp Treatment--The treatment for psoriasis of the scalp depends on the seriousness of the disease, hair length, and the patient' s lifestyle. A variety of non-prescription and prescription shampoos, oils, solutions, and sprays are available. Most contain coal tar or cortisone. The patient must take care to avoid harsh shampooing and scratching the scalp. Anthralin-- is a medication that works well on tough-to-treat thick patches of psoriasis. It can cause irritation and temporary staining of the skin and clothes. Newer preparations and methods of treatment have lessened these side effects. Vitamin D--A synthetic Vitamin D, calcipotriene, is now available in topical prescription form. It is useful for individuals with localized psoriasis and can be used with other treatments. Limited amounts should be used to avoid side effects. Ordinary Vitamin D, as one would buy in a drug store or health food store, is of no value in treating psoriasis. Calcipotriene is a synthetic form of vitamin D3 used for treating mild to moderate psoriasis. Sold as Dovonex in the U.S., this prescription medication is available in a cream, an ointment and a scalp solution. It is not known for working quickly, but it is effective and safe for long-term control of psoriasis, with few side effects. Dovonex is often prescribed in combination with other therapies, including topical steroids and ultraviolet light B (UVB). The drug is not recommended for treating psoriasis on the face, and it can cause temporary skin irritation. To avoid the medication being absorbed internally, people are advised not to use more than 100 grams of Dovonex cream or ointment or 60 milliliters of scalp solution in a week.
 Coal Tar--For more than l00 years, coal tar has been used to treat psoriasis. Today's products are greatly improved and less messy. Stronger prescriptions can be made to treat difficult areas. The Goeckerman Treatment is named after the Mayo Clinic dermatologist who first reported it in 1925. Combining coal tar dressings and ultraviolet light, it is used for patients with severe psoriasis. The treatment is performed daily in specialized centers. Ultraviolet exposure times vary with the kind of psoriasis and the sensitivity of the patient's skin. Light Therapy--Sunlight and ultraviolet light slow the rapid growth of skin cells. Though ultraviolet light or sunlight can cause skin wrinkling, eye damage, and skin cancer, light treatment is safe and effective under a doctor's care. People with psoriasis all over their bodies may require treatment in a medically approved center equipped with light boxes for full body exposure. Psoriasis patients who live in warm climates may be directed to carefully sunbathe. Seek the advice of a dermatologist before self-treating with natural or artificial sunlight. PUVA--When psoriasis has not responded to other treatments or is widespread, PUVA is effective in 85 to 90 percent of cases. This is offered at the local university, Loma Linda. The treatment name comes from "Psoralen + UVA," the two factors involved. Patients are given a drug called psoralen, and then are exposed to a carefully measured amount of a special form of ultraviolet (UVA) light. It takes approximately 25 treatments, over a two- or three-month period, before clearing occurs. About 30-40 treatments a year are usually required to keep the psoriasis under control. Because psoralen remains in the lens of the eye, patients must wear UVA blocking eyeglasses whenever using sunlight for illumination from the time of exposure to psoralen until sunset that day. PUVA treatments over a long period increase the risk of skin aging, freckling, and skin cancer including melanoma. Dermatologists and their staff must monitor PUVA treatment very carefully.
Coal Tar--For more than l00 years, coal tar has been used to treat psoriasis. Today's products are greatly improved and less messy. Stronger prescriptions can be made to treat difficult areas. The Goeckerman Treatment is named after the Mayo Clinic dermatologist who first reported it in 1925. Combining coal tar dressings and ultraviolet light, it is used for patients with severe psoriasis. The treatment is performed daily in specialized centers. Ultraviolet exposure times vary with the kind of psoriasis and the sensitivity of the patient's skin. Light Therapy--Sunlight and ultraviolet light slow the rapid growth of skin cells. Though ultraviolet light or sunlight can cause skin wrinkling, eye damage, and skin cancer, light treatment is safe and effective under a doctor's care. People with psoriasis all over their bodies may require treatment in a medically approved center equipped with light boxes for full body exposure. Psoriasis patients who live in warm climates may be directed to carefully sunbathe. Seek the advice of a dermatologist before self-treating with natural or artificial sunlight. PUVA--When psoriasis has not responded to other treatments or is widespread, PUVA is effective in 85 to 90 percent of cases. This is offered at the local university, Loma Linda. The treatment name comes from "Psoralen + UVA," the two factors involved. Patients are given a drug called psoralen, and then are exposed to a carefully measured amount of a special form of ultraviolet (UVA) light. It takes approximately 25 treatments, over a two- or three-month period, before clearing occurs. About 30-40 treatments a year are usually required to keep the psoriasis under control. Because psoralen remains in the lens of the eye, patients must wear UVA blocking eyeglasses whenever using sunlight for illumination from the time of exposure to psoralen until sunset that day. PUVA treatments over a long period increase the risk of skin aging, freckling, and skin cancer including melanoma. Dermatologists and their staff must monitor PUVA treatment very carefully.
Methotrexate is an oral anti-cancer drug that can produce dramatic clearing of psoriasis when other treatments have failed. Because methotrexate can produce side effects, particularly liver disease, regular blood tests are performed. Chest x-rays and occasional liver biopsies may be required. Other side effects include upset stomach, nausea and dizziness.
Retinoids--Prescription Vitamin A-related drugs may be prescribed alone or in combination with ultraviolet light for severe cases of psoriasis. Side effects include dryness of the skin, lips and eyes, elevation of fat levels in the blood, and formation of tiny bone spurs. Certain retinoids are not always used by women of childbearing age, as birth defects may result. Close monitoring is required with regular blood tests.
Biologics such as Enbrel, Humira, and Stelara are a new class of treatment for people with psoriasis and psoriatic arthritis. Biologic therapy offers needed new options for dermatologists and patients. Biologics are a class of drugs engineered from proteins produced by living cells; they disrupt the immune-system processes that drive the disease. Other treatments for psoriasis and psoriatic arthritis, particularly those used in moderate to severe cases, are effective but can have a widespread impact on the immune system. Biologic response modifiers are very helpful in the treatment of psoriasis. All psoriasis patients may benefit. Unfortunately, they are very very expensive, at upwards of $20,000 per course.
Cyclosporine : This drug, which suppresses the immune system, was originally developed to prevent the rejection of transplanted organs. Cyclosporine is approved for treating severe psoriasis in those people who cannot take or have not responded to other systemic therapies. It is available in either capsule or liquid form, which must be diluted for use. Cyclosporine generally works very well at improving or clearing psoriasis, and it is considered quick acting: results may be seen in as little as two weeks. However, cyclosporine has the risk of causing high blood pressure and damaging kidney function, and while these side effects are usually reversible if treated promptly, they are real and potentially serious. This medication is not approved for continuous treatment of more than one year.
What are the most common treatments?
- Topical corticosteroids are applied after removing scales by soaking in water. The ointment may be applied to wet skin, covered with a plastic wrap and left on overnight. During the day, topical corticosteroid creams are applied to the skin without coverings. Though topical cortisones are the most common medications used, prolonged application of topical corticosteroid creams may lead to atrophy of the skin, stretch marks, visible blood vessels, and skin discolorations.
- For very small plaques, triamcinolone acetonide may be injected directly into the lesions
- Anthralin preparations or coal tar preparations may give excellent results.
- If a strep throat infection is present, antibiotics may be used. This is most common in children.
- Scalp involvement may be treated with tar shampoos followed by corticosteroid lotions. If the plaques are thick, they may be removed before treatment with salicylic acid in mineral oil, covered with a plastic cap, and left on over night.
- Phototherapy with ultraviolet A or B light is often effective. Five minutes of direct sunlight each day will often help psoriasis.
- If conservative care fails, methotrexate may be used. It is one of the most effective treatments but it is potentially dangerous. Liver toxicity may occur with prolonged therapy. Increased risk factors for liver toxicity include a history of alcohol intake, abnormal liver function tests, IV drug use, and obesity. A pre-treatment liver biopsy may be required.
- Retinoids (Oral Soriatane) are sometimes used alone to clear resistant psoriasis, especially of the palms of the hands or soles of the feet. Retinoids may also be used in combinations such as with UVB. Retinoids may elevate the blood lipids in all patients, and may cause serious birth defects if given to pregnant women. They may remain in the body for 2 or more years. Topical retinoids are very helpful (Tazorac).
Tazarotene is a prescription topical retinoid (or vitamin A derivative) approved for treating mild to moderate plaque psoriasis. Sold in the U.S. under the brand name Tazorac, this medication is available in a gel in two strengths: 0.1% and 0.05%. It only needs to be applied once per day, and Tazorac can be used to treat scalp psoriasis and nail psoriasis, as well.
Tazorac can be prescribed by itself, but more and more dermatologists are prescribing it in combination with a topical steroid. The results are better, and the side effects are reduced—particularly the skin irritation that Tazorac can cause. The drug may also cause the psoriasis plaque to turn red before it clears, but this is a normal reaction and it will go away. 9. Biologics
The results of any of the above treatments are improved if the patient practices conscientious ABC moisturization. Ask Dr, Jacobs for the ABC booklet.
WHAT TO EXPECT
The prognosis for control is good following treatment. Scalp lesions may undergo remission for several months to years. For stubborn scalp psoriasis, you may try the P and S System. Please call: 800-735-2315 for further information. Some types of psoriasis persist for years and are characterized by unexplained remissions and exacerbations. The "Guttate" type of psoriasis may spontaneously disappear in a few weeks without treatment. Some benefits of treatment will come from the medications Dr. Jacobs prescribes, however, a great deal of improvement will come from your own daily care of your skin. Try to follow these guidelines and remain consistent with your therapy. WHAT MAKES PSORIASIS WORSE 1. Trauma and irritation to your skin: One of the most important points: Injury to or irritation of the skin may result in psoriasis. Rubbing, scratching, or scrubbing off scales, rubbing, brushing or picking at the scalp, sunburn, and local infection all can produce psoriasis. You should not scratch or rub your skin. The development of psoriasis after injury has been reported after surgical or accidental scars, burns, dermatitis (e.g. contact dermatitis as in poison ivy), bites, drug reactions, prickly heat rashes, sun rashes, seborrheic dermatitis, pityriasis roses, ringworm (fungus), thumb sucking, vaccination, herpes, shingles, and other infections of the skin. "Koebnerization" is the spreading of psoriasis after trauma. 2. Sun Exposure: Sunlight, in moderation, usually helps psoriasis but sunburn may cause psoriasis to flare up. A small percent (10%) of people may be made worse by any amount of sun. You should, therefore, use a sunscreen based on your skin type. Remember, for most people, five minutes of direct sunlight each day will often help psoriasis. 3. Infections: Sore throat and upper respiratory infections may flare psoriasis and should be promptly treated by your physician. Guttate (drop-like spots) psoriasis may occur in children and adolescents after strep throat activity. 4. Topical Steroids or Cortisone: Topical cortisones are very easy to use; however, if other medications are not added, then the psoriasis quickly returns. Topical cortisone should not be used on areas in which the psoriasis is cleared (when the skin is flat, even though it may be still a little brown). Misuse of topical cortisone, applying strong steroids (e.g. Temovate, Psorcon, Ultravate, Diprolene, Lidex, Halog, Synalar, Valisone) on skin too often and for too long a period of time can lead to changes in skin color, pimples, stretch marks, thinning of the skin, and easy bruising. Face and skin creases or folds (body folds) are in special danger for these adverse effects. Children are more prone to these adverse effects, so take care. 5. Other Drugs: Some drugs given for other diseases may make psoriasis worse. These may affect some but not all patients. Check with Dr. Jacobs. Drugs that may worsen your psoriasis include: Lithium, gold, indomethacin, beta-blockers such as Inderal, antimalarials, and Advil-Motrin like medications. Systemic steroids, such as prednisone, may clear psoriasis symptoms temporarily, but the psoriasis will return even worse when the steroid effect wears off. 6. Stress and Anxiety: Some patients find that stress makes their psoriasis worse. If this seems to occur try to find ways of stress control or reduction, such as relaxation programs. If stress remains a problem, then, counseling may be helpful. Call a counselor for help. You may find improvement for psoriasis through stress reduction.







